Recommendations for
Health Communicators:
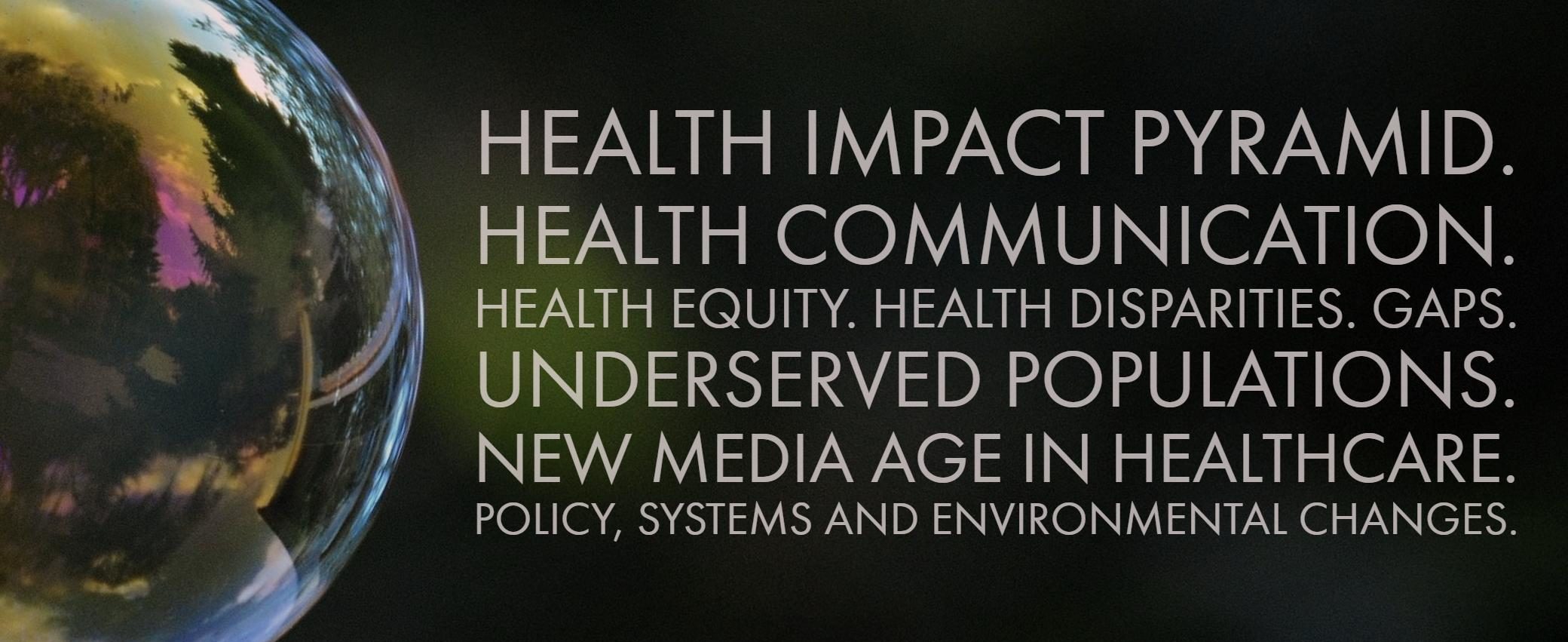
How to Close Gaps in Health Equity and Disparities Through Policies, Systems or Environmental Changes?
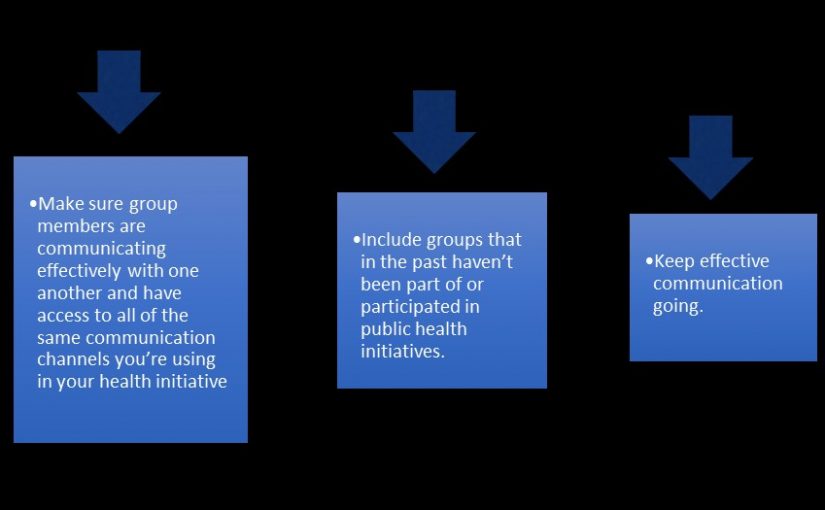
- Design and implement interventions with a focus on communities experiencing disparities.
- Actively engage representatives of communities experiencing disparities in all aspects of prevention strategies.
- Ensure that interventions are appropriate to the communities they are intended to support (e.g., using culturally relevant language, images, decision making, and communication processes).
- Strengthen the capacity of communities to enhance the likelihood of successful change.
- Engage community members in dialogue about health equity issues by providing workshops on digital storytelling to gather stories, empower community members, and promote positive health changes in the community.
- Then, invite local stakeholders to community meetings and forums where community members can showcase their videos and have a discussion.
- Create templates and worksheets to promote conversation among key stakeholders and community groups when carrying out meetings and health equity discussions.
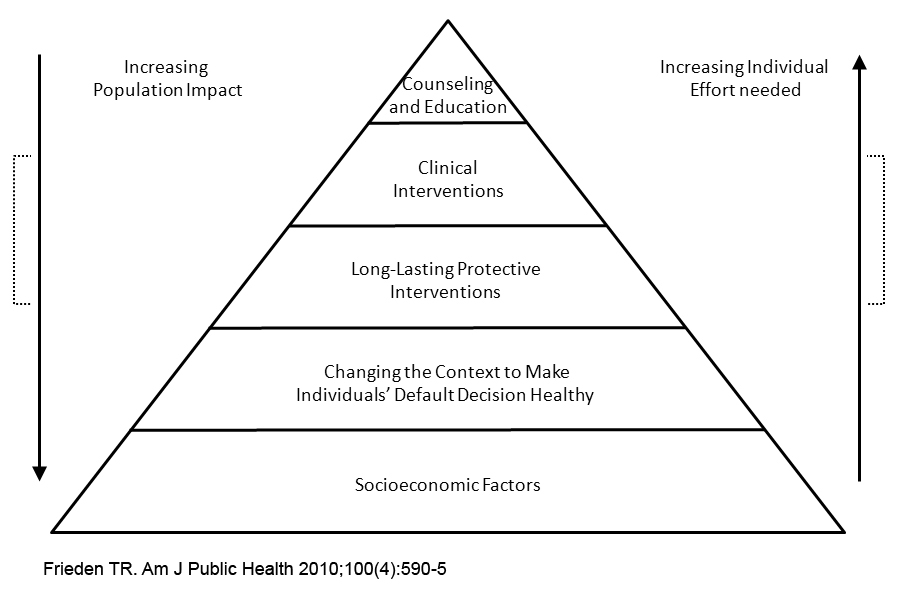
- Use policy, systems, and environmental change strategies that are sustainable and likely to reach large numbers of individuals and families while ensuring that these approaches do not widen health and equity disparities.
Continue reading Health Communicators Can Help Close Gaps in Health Disparities