What we’ve learned from the health impact pyramid is that by directing our efforts on community-wide health plans, we’ll have a better chance at generating more impactful and long-term outcomes on the health of people.
So, the base is representative of public health strategies directed at changing and enhancing the health of an entire population. This is where we would see the kinds of interventions that make the greatest impression on society’s health. That’s because these interventions are designed to reach a lot of people all at once, instead of one person at a time. Also, these responses ask for minimal effort from people as individuals.
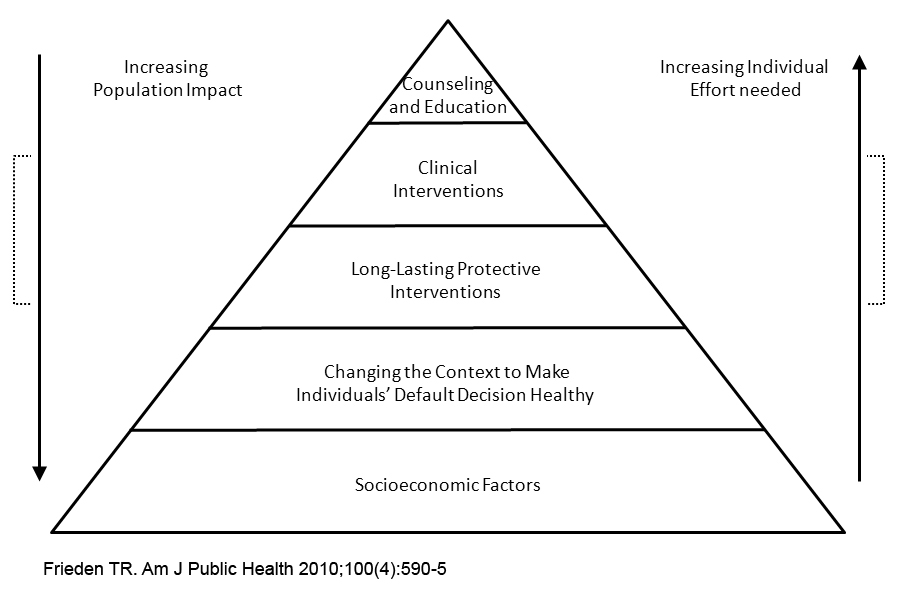
As we move up towards the top of the pyramid, the interventions have less impact because they’re mostly based on interventions that reach people on an individual basis, as opposed to the community as a whole.
Also, these interruptions (ahem, I mean interventions) require more effort on behalf of the individual.
In the middle, there’s a third level of the pyramid, which Frieden explains “represents 1-time or infrequent protective interventions.” [i]
That section reminds me specifically of the Theory Picker tool that we used in the last lecture. There’s a part where you identify whether the behavior you’re looking to change is a “Just a 1-time thing, not something that must be done over and over to benefit health or avoid a health risk.” [ii]
Everything intersects in the end.
So, when asking myself how health communication fits into the topic of health equity and disparities –well, I can say that the answer is exemplified using communication tools.
The phenomenon of using a theory picker to aid in the selection of the best possible intervention model, and in turn design an effective health initiative that’s subsequently implemented appropriately and efficiently, and delivers visible and measurable results —- that illustrates how health communications fit into the topic of health equity and disparities.
As health communicators, it is crucial to remember the following when addressing social determinants of health inequities: [iii]
► Make sure group members are communicating effectively with one another and have access to all of the same communication channels you’re using in your health initiative.
► Include groups that in the past haven’t been part of or participated in public health initiatives.
► Keep effective communication going.
With health communication, we can address specific factors when designing strategies to prevent health conditions, this results in maximizing health impact and advancing health equity.
Recommendations for Health Communicators:
How to Close Gaps in Health Equity and Disparities Through Policies, Systems or Environmental Changes? [iv]
- Design & implement interventions with a focus on communities experiencing disparities.
- Actively engage representatives of communities experiencing gaps in all aspects of prevention strategies.
- Ensure that interventions are appropriate to the communities they are intended to support (e.g., using culturally relevant language, images, decision making, and communication processes).
- Strengthen the capacity of communities to enhance the likelihood of successful change.
- Use policy, systems, and environmental change strategies that are sustainable and likely to reach substantial numbers of individuals & families while ensuring that these approaches do not widen health & equity disparities.
References:
[i] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2836340/
[ii] http://www.orau.gov/hsc/theorypicker/picker.html
[iii] https://www.cdc.gov/nccdphp/dch/programs/healthycommunitiesprogram/tools/pdf/SDOH-workbook.pdf
[iv] https://www.cdc.gov/nccdphp/dch/pdfs/health-equity-guide/healthequity_infographic_508.pdf