July 20. 2020 Important update on superspreading events.
This article from the Washington Post provides a useful update about how superspreading events account for the vast majority of infection and are driving the pandemic. 3-5 minute read.
Washington Post Ariana Eunjung Cha July 18, 2020 at 1:58 p.m. EDT
‘Superspreading’ events, triggered by people who may not even know they are infected, propel coronavirus pandemic
https://www.washingtonpost.com/health/2020/07/18/coronavirus-superspreading-events-drive-pandemic/
I also enjoyed the very accessible video link on the science of COVID-19 which is linked on the first page of this article. (4 minutes.) I could not copy just its link…
The novel coronavirus is a master of disguise: Here's how it works
All is well in my household. Wishing you the same. Randy
July 5, 2020 Hopeful news on speedy SARS-COV-2 testing!
The US federal government is doing a terrible job at tracking cases compared to many other countries. But if some of the fast, low cost technologies for individual testing mentioned in this NY Times Opinion piece actually work, it will make it a lot easier for individuals, schools, firms and motivated local governments to do so. The lead author is BU professor of economist. (5 minute read)
With easy-to-use tests, everyone can check themselves every day.
By Laurence J. Kotlikoff (BU) and Michael Mina (HSPH), July 3, 2020
June 20, 2020 COVID-19 recovery
By Carrie MacMillan, Yale University,
June 19, 2020
Yale Medicine physicians describe the recovery path they’ve seen for patients experiencing 'mild to moderate' forms of the disease.
RE: I would have liked more details about the recovery of people who have more serious forms of COVID-19. This report from Kaiser Health News provides one such glimpse.
June 17, 2020 Honor roll of favorite COVID-19 web sites
I often blog about the most recent studies and news reports of interest, but usually it is worth focusing on the best ones. Below is my honor roll of favorite links on COVID-19, all from below.
Sources we're following. Updated weekly blog by Vivian Ho and staff at the Baker Institute of Public Policy at Rice University
COVID-19: An illustrated scientific summary 8 minute video by a Yale graduate student gives an excellent overview.
The Risks - Know Them - Avoid Them, by Erin S. Bromage, Ph.D.
Tomas Pueyo's March 19 article in the Medium: Coronavirus: The Hammer and the Dance. Dance sequel articles, full of figures are linked here (warning: long, meaty reads).
The best up-to-date statistics on COVID-19 is WorldoMeter.info/coronavirus.with daily updates and documented sources.
New York Times interactive figures are updated regularly for the countries of the world and individual US states and are still the best to me, using log scales.
Covidtracking.com summarizes raw data on COVID-19 for the US, and now includes a new tracking of cases and deaths by race.
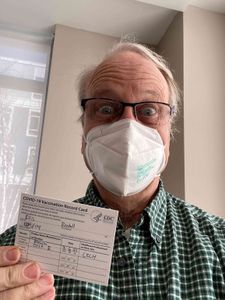
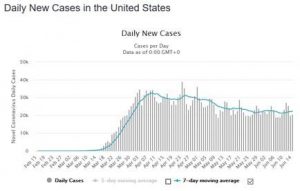
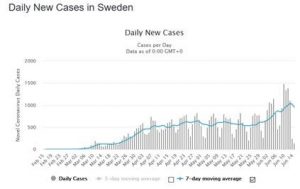
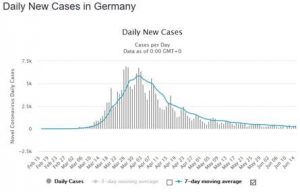
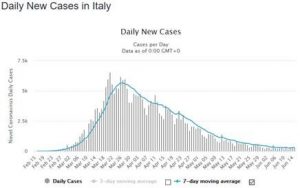
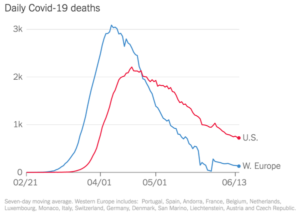
July 17, 2020 Western Europe versus US
Just out from the New York Times.
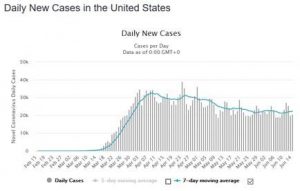
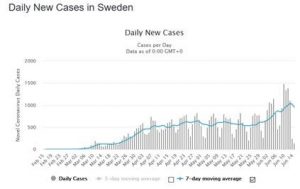
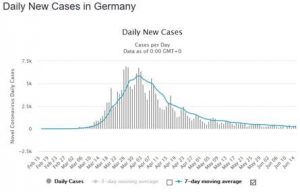
June 17, 2020 Current trends in cases around the world.
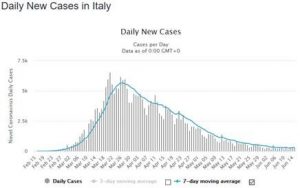
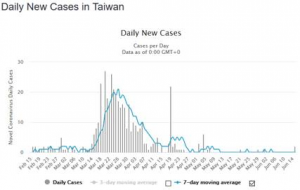
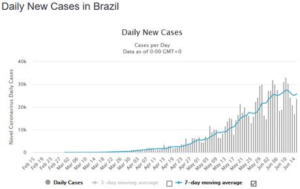
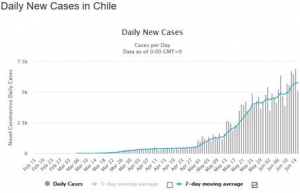
Below are charts from 6/16 from WorldoMeter.com/coronavirus for a set of countries I am tracking. Each figure has a story. You can decide for yourself which ones you like.
(Yes, I prefer tracking deaths, but there is also a bias to deaths as well, plus deaths lag reported cases by about two weeks (~12 days), and the last two weeks are informative in many countries, including the US and elsewhere. Rates of testing tend to change only slowly.)
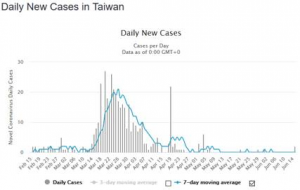
Note that unlike the above, the Taiwan cases is not in hundreds or thousands. (Population 23 million)
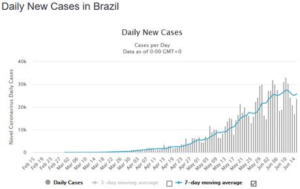
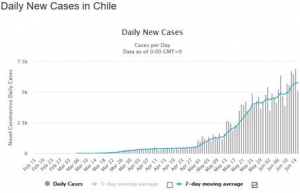
It is the start of winter in most of Brazil and Chile. Not a good omen for this fall in the North.
June 17, 2020 World War I and II comparisons
Today’s Boston Globe features the news that COVID-19 deaths in the US – currently 119,000 – now exceed those in World War I. Of course the US population was much lower then. During World War II there were 407,316 service men who died (0.29 percent of the US population). Think of all those flags for WWII veterans you saw on Memorial Day recently. It will take real determination and action to keep US deaths from COVID-19 – currently about 800 per day, or 24,000 per month – below the tragic WWII levels.
June 17, 2020 Be selfish and wear a mask!
Yesterday I ate dinner outside on the main thoroughfare (Moody Street) in Waltham which has been converted into a massive pedestrian way to allow people to eat outside while more than 3 meters apart. I was sad to see dozens of people on the streets not properly wearing masks. I thought of a good selfish reason why everyone should want to do so. Just as high altitude dwellers develop stronger and larger lungs in order to get enough oxygen, securely wearing a high quality mask that cuts off the air flow a bit and results in slightly less oxygen reaching your lungs enables low altitude people to develop stronger and larger lung capacity. The extra effort it takes to breath is no different from lifting more weights or running a bit faster, and builds up your lungs at a time when you may really need them to fend of COVID-19 respiratory failure. I don’t hear weightlifters or joggers complaining about their difficulties: they want the challenge. Wear a high quality mask for your own future health!
June 11, 2020 Words from Michael Osterholm, epidemiologist
I am sharing this informative interview with a very knowledgeable person, even though I disagree with his assessment on several important points.
I have added my comments at the bottom of this summary from the article, while striking out three statements asserted there.
COVID-19: Straight Answers from Top Epidemiologist Who Predicted the Pandemic
https://www.bluezones.com/2020/06/covid-19-straight-answers-from-top-epidemiologist-who-predicted-the-pandemic/
By Dan Buettner, Blue Zones Founder [Interview conducted on May 29, 2020. Published on June 6, 2020]
Below is the summary from within that article.
In short, Dr. Osterholm is arguably one of the most dependable, non-political sources for straight answers on what COVID-19 means to us and our world in the immediate future. In his 2017 book, Deadliest Enemy, he correctly foretells a global pandemic and offers the best strategy for fighting it now and avoiding it in the future.
Here are the highlights of our conversation. But if you really want to understand this disease, read the whole interview. This disease may be the biggest event of our lifetimes.
- 3 months ago, COVID-19 was not even in the top 75 causes of death in this country. Much of the last month, it was the #1 cause of death in this country. This is more remarkable than the 1918 Flu pandemic.
- There is no scientific indication Covid-19 will disappear of its own accord.
- If you’re under age 55, obesity is the #1 risk factor. So, eating the right diet, getting physical activity, and managing stress are some of the most important things you can do to protect yourself from the disease.
- One of the best things we can do for our aging parents is to get them out into the fresh air, while maintaining physical (not social) distancing.
- Wearing a cloth mask does not protect you much if you’re in close contact with someone who is COVID-19 contagious. It may give you 10 minutes, instead of five, to avoid contracting the disease.
- We can expect COVID-19 to infect 60% – 70% of Americans. That’s around 200 million Americans.
- We can expect between 800,000 and 1.6 million Americans to die in the next 18 months if we don’t have a successful vaccine.
- There is no guarantee of an effective vaccination and even if we find one, it may only give short term protection.
- Speeding a vaccination into production carries its own risks.
- The darkest days are still ahead of us. We need moral leadership, the command leadership that doesn’t minimize what’s before us but allows everyone to see that we’re going to get through it.
I strongly disagree with his statement that wearing a cloth mask does not protect you much. It is true that if I were tending a COVID-19 infected patient, it would be highly inadequate, because of the duration of the exposure. But for ordinary activities, even briefly near someone who is infected, then universal mask wearing by both the infected and the rest of the population can bring down the rate of new infections below 1.0, and largely eliminate or drastically slow down exposure in a population. This is why New Zealand has had zero deaths over an extended period, and why rates are also extremely low in Japan, Hong Kong, South Korea and certain other Asian countries. All of these countries have had nearly universal mask wearing, as well as excellent case identification and quarantining.
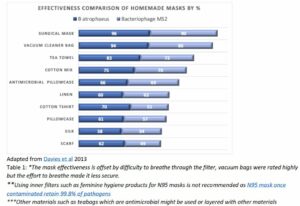
The research on masks shows that a simple, homemade cotton mask filters out about 70% effective at suppressing germ aerosols, particularly larger particles that can projectile the farthest from a sneeze, cough or singing. Masks also reduce touching your mouth, nose and eyes, even if they don’t eliminate any aerosol contamination. Better “surgical quality" masks can achieve over 95% protection with 99% claimed by N95 masks. (To some degree, the greater risk may be putting on and taking off high quality masks frequently to maintain their effectiveness…) There is no reason we could not all be wearing surgical quality masks when shopping or around others. This would greatly slow down transmission.
If a random COVID-19 contagious person without any PPE protection infects 3 people, then even a 70% effective mask reduces the average number of people infected to .3*3 = .9 newly infected for each person contagious. That is less than 1! So the disease would gradually die out. With a 90% effective PPE, new infection rate would be cut to less than a third, and infections would die out even faster.
PPE is why in Japan millions of people are now commuting daily by public transport on crowded subways and buses with minor numbers of new cases: masks do work. We could do that if we all wore masks, testing was widespread, and we were willing to track cases and enforce quarantines.
I also disagree with the papers blind prediction that COVID-19 will necessarily infect 60-70 percent of the worlds population. The same experience from other countries show that careful testing quarantining, and mask wearing could keep rates below 60% of the population, particularly the at-risk population, for over a year, when hopefully a vaccine will be available for at least high risk people. Recall that until a few years ago flu vaccines were reserved only for older and higher risk segments of the population. This is what will be needed this time as well, when a COVID-19 vaccine is created, since we cannot immediately create 8 billion vaccines for the whole world.
The article starts with a really crazy statement:
“One of the things we have to understand is that this virus is operating under the laws of physics, chemistry, and biology. It doesn’t in any way, shape, or form bend itself to public policy.”
If it were true that science drives everything and public policies do not matter, then why do we even need doctors and hospitals? Or why does physical distancing matter? Clearly public policy AND PRIVATE DECISIONS matter a lot, as the article goes on to highlight.
I agree that each country needs a leader like Franklin Delano Roosevelt who is unselfish and totally committed to leading the public sentiment in a positive direction. A few countries have been blessed with this, and we should be learning from their successes.
My own wish is that more attention would focus on the following facts.
- The death rate is not some constant for each health care system, but rather it will go up if a health care system gets overcrowded and cannot keep up. It could be that with optimal treatment in a well-endowed health care system, the death rate is only 0.5% of those infected (across the whole population). But if there are not enough hospital beds, trained doctors, staff, ICUs and ventilators, then the death rate could be 5%. This is the great value of policies to slow down rates of infection.
- A significant part of the burden of high rates of COVID-19 is the consequences of all the avoided preventive and curative treatment of OTHER diseases. Heart conditions, cancer, vaccine preventable infections. This is another reason to want to keep the flow rate of new infections manageable.
- While everyone is focusing on when there will be a vaccine, of greater likelihood is that we will develop treatment strategies that can further reduce mortality and serious illness. This is what is more likely in the near term.
- I think it is too early to tell whether death rates by the rest of the world are much better than in Sweden, which has encouraged private actions but not shut down and mandated self-quarantines. We have so far DELAYED infections and deaths meaningfully in the US and many other countries, but whether we have prevented them over say the next year will depend on what happens this fall and winter.
- There is far too little effort and research discussing how to better target social distancing and public polices to people at greatest risk. Shutting down all businesses is a very blunt tool for doing this.
- The findings that high altitudes have lower rates of infection is likely not the result of the virus not finding conditions less hospitable at low air density or humidity, but rather that at high altitude people develop larger lungs and stronger lung muscles that make them better able to fight off the virus. Working out hard can do much the same thing for many of us.
- Obesity affects heart and circulatory diseases in part because the fat clogs up arteries and veins. For COVID, a different mechanism may be that obesity increases the weight that the lung muscles have to raise and lower with each breath, which leads to faster respiratory failure and requires the really nasty ventilators that replace muscles and cause all kinds of problems of their own. We all know that repeatedly raising your arms while holding even a one pound weight soon wears your arms out. The same must be true for breathing with extra pounds of weight on your chest and stomach. The shrotness of breath symptom of COVID-19 can force you to breath hard for hours or days at a time.
- There is evidence in JAMA just out from China that shoes spread around germs all over the floor when people walk in areas around infected people, even if those people are not showing any symptoms. Most of us don’t touch the floors much, but infants do. While symptoms are concentrated among the old populations, US studies show that infection rates are pretty uniform across all ages. Parents should not let very young children crawl on floors in public places.
- Teens and college age students are especially prone to large gatherings (sports, concerts, bars,…) in which people mingle with strangers, and many infected do not display symptoms. While serious cases are rare, they are also likely to be a very strong source of new infections.
Randy Ellis
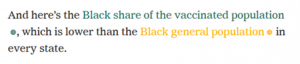
June 8, 2020 More on Race and likely futures
Covidtracking.com is an new source of raw data on COVID-19 statistics for the US, and now includes a new tracking of cases and deaths by race.
This source is the new standard being quoted by the media, including by the White House and CDC. I have not compared it to the NY Times and WorldOMeters.com sources that I have previously linked.
I am not sure I agree with the consensus, but this survey out just today of epidemiologists by the NY Times gives a very sobering overview of when we might expect to return to a wide range of normal activities.
https://www.nytimes.com/interactive/2020/06/08/upshot/when-epidemiologists-will-do-everyday-things-coronavirus.html
June 5, 2020 Repost of Austin Frakt's "An open letter to White people."
An open letter to white people
May 28, 2020
What’s the Risk of Catching Coronavirus From a Surface?
NY Times 5/28/2020
RE: This is a reassuring article to me. We should not become paranoid over the very low risk of contamination from touching surfaces, which is dealt with effectively by frequent hand washing. (Three minute read.)
https://www.nytimes.com/2020/05/28/well/live/whats-the-risk-of-catching-coronavirus-from-a-surface.html
May 21, 2020 more from the U Mass Dartmouth biology professor.
Erin Bromade PhD. has an excellent 4 minute CNN interview on outdoor barbecues, shared bathrooms for dinner guests, and swimming pools. With his Australian accent, it is a fun listen. Very specific. Watch it here.
May 21, 2020 Steps hospitals use to minimize COVID-19 and more
Excellent article by Atul Gawande in the NYTimes magazine. Probably a 20 minute read.
Key takeaways for me:
"Is there any place that has figured out a way to open and have employees work safely, with one another and with their customers?" Yes. Mass General Brigham, ... seventy-five thousand employees—more people than in seventy-five per cent of U.S. counties. In April, two-thirds of us were working on site. Yet we’ve had few workplace transmissions. Not zero: we’ve been on a learning curve, to be sure, and we have no way to stop our health-care workers from getting infected in the community."
"Its elements are all familiar: hygiene measures, screening, distancing, and masks."
"The SARS-CoV-2 virus does not last long on cloth; viral counts drop ninety-nine per cent in three hours."
"Toughing it out is now a shameful act of disloyalty."
"Surgical masks are made of a melt-blown polypropylene fibre fabric, which, under magnification, looks like cotton candy. Most of the filtration this material provides isn’t from direct blockage but from an electrostatic charge applied to the fibre using a machine called, aptly enough, a corona charger. The static electricity captures viral particles the same way that a blanket in the dryer catches socks. This allows the material to breathe more freely. Cloth masks feel warm and smothering by comparison, and people tend to loosen them, wear them below their noses, or take them off more frequently. The fit of improvised masks is also more variable and typically much worse. A comparison study found that surgical masks did three times better than homemade masks at blocking outward transmission of respiratory viruses."
I also enjoyed the following link on the value of face masks. The comments on this are indicative of how a strong, well organized contingent in the US is arguing against masks.
As before, Vivian Ho's weekly blog is full of many great links. Including recent work by Erin Bromage.
May 21, 2020 Sad humor: some governments are distorting with statistics.
See this post on Andrew Gelman's blog. Ten minutes. See if you can see what is wrong.
https://statmodeling.stat.columbia.edu/2020/05/18/hey-i-think-somethings-wrong-with-this-graph/
https://statmodeling.stat.columbia.edu/2020/05/16/what-a-difference-a-month-makes-polynomial-extrapolation-edition/
May 16, 2020 New Favorite overview of the Dance challenges
Way back on March 29 I recommended Tomas Puyea EXCELLENT, clairvoyant article
Coronavirus: The Hammer and The Dance (29 minutes).
That article is foundational and is still be essential reading for everyone.
I have been remiss in not revisiting and following Puyea's subsequent work, which contains an excellent Learning How to Dance series. He has just released Part 5. I recommend all of them, although there is some overlap, as there should be in any "Learning how to..." series.
Part 1: Coronavirus: Learning How to Dance (19 minutes)
Part 2: Coronavirus: The Basic Dance Steps Everybody Can Follow (18 minutes)
Part 3: Coronavirus: How to Do Testing and Contact Tracing (39 minutes)
Part 4: (not yet published)
Part 5: Coronavirus: Prevent Seeding and Spreading (31 minutes)
Key insights from all of this:
We should particularly avoid allowing very large gatherings such as sporting events, conconcerts, crowded churches, restaurants with no spacing, because these are the worst hazards to the Dance.
Several countries have successfully quashed the infections, but will have to continue to restrict outside visitors and even regional travel.
Some countries and some US states have taken few precautions and will end up needing to get to herd immunity to stop the spread. This will take about two thirds of the population getting ill before infections quiet down, at a fatality rate of .5 to 1.5 this would kill 1 to 3 million Americans. there are many excellent figures and simulations that highlight all that can be done without totally closing down the economy
28 percent of infected people infect their spouses, 14% infect other people they live with, and 4% infect their children. Social distancing within the household is very challenging.
Opening schools while managing interactions to be only among smaller groups and having monitoring is proving successful in many countries.
South Korea never really shut down, but has extraordinary public effort, public information and intrusive quarantining.
International and even regional travel will likely have to be restricted for a very long time, such as until an effective vaccine.
There is still no guarantee that a vaccine or immunity will be effective for more than two years.
My own thoughts to add: There is very little in Puyeas work about the role of weather. Colder, drier areas do seem to have greater exposure.
I see a great need to highlight that even vacation travelers can stay in hotels and summer rental housing if they are willing to leave an interval of 3-4 days between guests. Similarly mail, store purchases, and food, that has not been touched for a few days is inherently safe. Things stored outside in UV light including picnic tables and benches and rocks and trees are also extremely low risk because of this natural healing.
The findings discussed in Erin Bromage (see May 11 blog summary below) that only 0.3 percent of all infections have been traced back to someone getting infected outdoors speaks volumes to me.
We will have to give up not only handshaking, but also hugs, social kisses, and close encounters among family and friends. Italian and Spanish traditions, young people in clubs and others who believe in extensive close social contacting will need to change.
The latest antibody test in the city of Boston found that about ten percent of the population has been infected so far. So Boston is about 1/7th of the way to herd immunity.
COVID-19 antibody test results from Santa Clara (1.5% of population testing positive), and from Denmark (1.8%) taking antibody tests of random samples find that overall infections are approximately uniform by age. Children are just as likely be become infected as adults, but they are much less likely to show symptoms or become highly contagious.
Future costs of all the medical complications of people who recover from COVID could be very serious.
I can't resist including an extended quote describing Taiwan's response to COVID in March. This is taken from Part 1. All highlights were in the original article. They have only had ~500 cases and 46 deaths so far. Population is 24 million, more than New York State (19 million). Enjoy.
"Taiwan’s level of preparedness is jaw-dropping. This is a list of over 100 measures they took before March. Here are some examples, from the list and other sources:
- Early and strict travel bans, updated every day.
- They centralized the management of mask production, starting at 2.4 million per day (twice their need of 1.3 million at the time).
- They set the price to avoid profiteering, initially at USD $0.50 per mask.
- The penalty for price gouging for masks and other key items became 1–7 years in jail and a fine up to USD $167,000.
- The spread of fake news could be fined with USD $100,000.
- Proactive detection of cases: They tested all people who had previously had flu symptoms but tested negative for flu, finding some coronavirus patients.
All of the above happened BEFORE Wuhan even shut down! Then, they continued:
- Soldiers were mobilized to produce masks.
- The official price of masks was eventually down to ~$0.20 by the end of February.
- Eventually, they ramped up production to 10 million masks per day (for a population of 23 million) before the end of March. Masks were rationed and their export banned.
- Travel and healthcare databases were connected, so healthcare professionals could know who was at a higher risk of being infected. The Taiwanese CDC could track what was happening on the field in real time.
- It triaged travelers based on their risk, from free to enter the country with self-monitoring to mandated quarantines.
- Quarantine support with food and encouragement.
- Enforcement of the quarantine through people’s existing phone signals. If they don’t have a phone, the government provides them with one. An alert is sent to the authorities if the handset is turned off for more than 15 minutes.
- Persons who were not compliant with home quarantine orders were turned over to law enforcement and tracked by police officers. A couple was fined USD $10,000 for breaking the 14-day home quarantine rule.
If the world was a class and each country was a student passing a coronavirus exam, Taiwan is acing the test. And it’s offering to help. If I were another student, I would take that offer.
That it for now.
May 13, 2020 Hopeful article about the search for effective drugs
By Kim Tingley, New York Times, Published May 13, 2020
The article highlights the extraordinary level of cooperation internationally, as well as the dangers of the US claims that China is stealing US secrets. This is not a time for the US to interfere with science because of worries about who makes the billions of dollars a new drug will be worth.
May 13, 2020 A not so welcome reminder
New York Times Interpreter by Max Fisher and Amanda Taub
It reminds us that the successes of South Korea and China were "test, trace, and mandatory quarantine with fines" and not just "test and trace."
May 11, 2020 Hot off the presses from U.Conn., MIT-Sloan Harvard, and collaborators
Weather Conditions and COVID-19 Transmission: Estimates and Projections
Ran Xu, Hazhir Rahmandad, Marichi Gupta, Catherine DiGennaro, Navid Ghaffarzadegan, Mohammad Jalali
The attached paper was just posted today on SSRN with coauthors from UConn, MIT-Sloan and Harvard. It has over-the-top modeling of daily data from every county in the US, plus cities, states or countries worldwide rates of COVID-19 infection based on weather, humidity, air pressure, geography, wind, sunlight, and even the phases of the moon! (This last one has to be considered the werewolf effect, which they omitted from their final model even though statistically significant.) I saw the write up about it in the Boston Globe yesterday but the actual paper was only posted on May 11.
https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3593879
They do not forecast rates of disease but only relative rates of infectiousness and how they are affected by weather. They have only a few months of data from a wide range of worldwide cities.
They have a really cool graphics generated here, including the ability to generate weekly forecasts of relative rates of infectiiousness by city, county state and country worldwide. You can play with it to look at patterns by state, simulated by week across the year.
https://projects.iq.harvard.edu/covid19/us-counties
They get that favorable weather can reduce rates of infection by about 40 percent, or worsen it by about the same. Given that the rate is about 2 overall, then this means it will slow down in many parts of the US this summer, but then come back strong next fall or winter. It is worse in cold, dry areas.
May 11, 2020 Best overview of COVID infectiousness
I have read a lot of articles about COVID, but this paper, by a professor of biology of U Mass Dartmouth, is the best so far at signalling how different activities and situations vary in their riskiness. I recommend it highly to everyone.
The paper emphasizes
Successful Infection = Exposure to Virus x Time.
Shopping in an uncrowded large store for a short time is relatively safe, as is jogging and brief contact while social distancing. In contrast indoor in-person meetings, especially in small areas, parties, church gatherings, concerts or other large gatherings, or other events that last for an hour or more and include talking, singing, eating, exercising, or touching shared items are the most risky.
Here is the direct link. It is a 12 minute read. Do it now!
I especially like that this article is by an ordinary professor, who has just done an extraordinary synthesis of German case studies, epidemiology and other diverse scientific sources. It highlights that all of us can play a role in fighting this virus.
Also, I also recommend this article by the same author, which covers events in China, the origins of the virus, and descriptions of various tests and vaccines.
https://www.erinbromage.com/post/where-we-are-now
About the author:
Erin S. Bromage, Ph.D., is an Associate Professor of Biology at the University of Massachusetts Dartmouth. Dr. Bromage graduated from the School of Veterinary and Biomedical Sciences James Cook University, Australia where his research focused on the epidemiology of, and immunity to, infectious disease in animals.
May 9, 2020 Good signs.
Today (Saturday) I ventured out out to a local hardware store to get a few gardening items and to CVS to pick up a few health items. Among the many encouraging signs were:
- Everyone I saw in either place was wearing a mask,
- Social distancing was marked on the floor and adhered to.
- CVS was actually selling nursing quality masks (not N95, but at least with metal strips around the nose) for $2 apiece, limit of 4
- The hardware store was selling hand sanitizer and bulk packages of 100 gloves at a normal price.
- Everyone was friendly and happy.
There is hope for a more pleasant existence in our future together, even if things will remain different for a while now. Keep your hopes up!
May 8, 2020 Careful statistical model of COVID-19 fatality rates
Anirban Basu, an exceptional econometrician (with 9252 Google Scholar citations) at the University of Washington who is personally known to me, published an article that just appeared in Health Affairs yesterday.
Using daily county-level data on deaths and new cases from the US up through April 20, 2020, he estimates Bayesian models of the infection fatality rate among symptomatic cases (IFR-S) which give a point estimate of 1.3% of all people with COVID-19 symptoms dying.
The Health Affairs article is heavy reading for a non-statistician. To give you a flavor, here is the key sentence about methodology: "The mean of this Binomial model, p_jt, represents the probability of death, and is expressed as a Bayesian random-coefficients exponential decay model within a logit link framework so that the predicted rates remain within 0 and 1."
Here are the first few sentences from the abstract.
"ABSTRACT: Knowing the infection fatality rate (IFR) of SARS-CoV andSARS-CoV-2 infections is essential for the fight against the COVID-19 pandemic. Using data through April 20, 2020, we fit a statistical model to COVID-19 case fatality rates over time at the US county level to estimate the COVID-19 IFR among symptomatic cases (IFR-S) as time goes to infinity. The IFR-S in the US was estimated to be 1.3% (95% central credible interval: 0.6% to 2.1%). County-specific rates varied from 0.5% to3.6%. The overall IFR for COVID-19 should be lower when we account for cases that remain and recover without symptoms."
This segment was also highly informative to me.
"Results from sero-testing from the Diamond Princess outbreak suggests that about 17.9% of infected persons never developed symptoms.10 Consequently, a reasonable estimate of the overall IFR would be about 20% lower than our estimated IFR-S."
In the conclusion:
"If we carry out a thought experiment where 35.5 million individuals would contract COVID-19 illness this year in the US (i.e., the same number as flu last year)19 then, in the absence of any mitigation strategies or social distancing behaviors and the supply of health care services under typical conditions, our IFR-S estimate predicts that there would have been nearly 500,000 COVID-19 deaths this year. To the extent that COVID-19 is more infectious than flu and does not have any protection from a vaccine or treatment, the number of infections, and hence the number of deaths, would be higher. Certainly, with mitigation strategies, the death toll will be lower."
My interpretation: The paper is very open about biases upward and downward. One bias not discussed is the number of deaths unreported in the data, which now appears to be significant. Death rates in the US are likely to be higher than in other countries, for many of the reasons discussed in the Boston Globe article linked here. Still, these are very sobering numbers for the US.
May 7, 2020 - EXCELLENT Boston Globe article on diet and its link to COVID-19.
Many COVID-19 hospitalizations, ICU admissions, and deaths could be prevented if Americans had a better diet and better metabolic health.
By Mark Hyman and Dariush Mozaffarian Updated May 7, 2020
Here are a few key sentences (with cites) from the article that resonate with me.
"Ninety four percent of deaths from COVID-19 are in those with an underlying age-related chronic disease, mostly caused by excess body fat."
"Only about 12 percent of Americans are metabolically healthy, without a large waist, high blood pressure, high blood sugar, or high cholesterol."
"The sad reality is that 75 percent of Americans are overweight, and more than 42 percent are obese. Chronic disease affects 6 out of 10 Americans. Also 20 percent of normal-weight people have prediabetes. These shocking rates of poor metabolic health — with nearly 9 out of 10 American adults unhealthy — is a major reason the COVID-19 crisis is so much greater than it needs to be."
My interpretation: Just like a marathon race, winning against the coronavirus requires a strong immunity system, strong lungs, and a healthy heart. Americans, and particularly poor Americans, are compromised in all three with their diet, lifestyle and environment more than the rest of the world. I invite you to read the article.
Fortunately, for many of us with increased free time, the inconvenience of buying large quantities of food, and greater motivation, now is a good time to do something about it.
May 1, 2020 NY Times links below are useful for data updates.
As May begins, stay-at-home orders end
Governors of coastal states including California and Florida have faced particular pressure as they try to balance health concerns with growing demands for beach access as the weather heats up. Here’s a map of the varying restrictions across the U.S.
Gov. Gretchen Whitmer of Michigan reinstated a state of emergency on Thursday, even as protesters, some of them legally armed, gathered at the State Capitol.
Here are the latest updates from the U.S. and around the world, as well as maps of the pandemic.
For a detailed picture of the outbreak in the U.S., we’ve also compiled data from hundreds of metro areas.
May 1, 2020. Pessimistic forecast from Yahoo Finance, and my own thoughts.
Here is an insightful interview with El Erian on the monetary and fiscal responses to COVID-19:
https://finance.yahoo.com/video/el-erian-worst-recession-since-154048623.html
His statements accord with my view. Pretty grim.
The most telling thing to me is the lack of confidence and incredibly negative consumer expectations. People are only buying necessities, and that will not fuel the economy. Even food production (meat, fresh vegetables) is now uncertain. On April 10, a poll of sports fans found that 72% would not plan to go to a sporting event even if they resume in September. (What about children in schools or universities or any public entertainment, or restaurants?) Even the workers getting government aid want to save it since they realistically fear that the worst is yet to come. The ridiculous epidemiological model from U. Washington predicting a nice bell-shaped declines in rates of infection with the shutdown are not even close to the persisting rates of new cases, and the very gradual, flat persistence. Deaths are being grossly undercounted, and we are still less than 10% of the way toward herd immunity. Reopening the economy fully will I believe likely cause many areas to overload their hospital capacity in about three weeks: the average time from new infections to death (two to three weeks) plus a week for a renewed doubling in cases because we still have high fundamental infection rates to start from.
I am not a macro economist, but we now have a shock where earned income has dropped about 40% (Ellis and Marcolongo, April 17, 2020, with a new draft out next week), and more in the most vulnerable occupations. Current PPP loans are not reaching the neediest, and $1200 per person will not last long. Cities and states will soon be going bankrupt and start having to lay off public workers unless the federal government acts very quickly, which they can’t. Even people who have income, like me, are perhaps spending less than half of what they would usually spend, hording food, but not spending anything on travel, transportation, other consumables or durable goods. We are just spending more on personal delivery services and internet services. Health care spending will be strong, however, given the resources spent on COVID, but offset by canceling most elective and preventive care. I can easily see a more than 50% decline in consumption spending in the economy. Something similar is happening in the rest of the world, plus trade is also collapsing. I don’t see why the stock market is still acting like we will come out of this quickly. (Remember, the Dow Jones lost 75% of its value in the Great Depression. We are a long way from that now.) The economy is so dreary that I have pretty much stopped blogging about my predictions in the last week.
I am enjoying bird photography, vegetable gardening, and baking bread. I recommend these activities highly to you. It is nice to fall asleep thinking about gardening or how to zoom about birds instead of about COVID-19.
The state of Maine started reopening as of today. Lets see what happens.
Have a good weekend!
Randy
April 23, 2020 Science article about COVID-19 effects
This Science article has an excellent overview about the complex medical challenges from COVID-19.
I recommend it to anyone interested in clinical manifestations, rather than economics or epidemiology.
How does coronavirus kill? Clinicians trace a ferocious rampage through the body, from brain to toes
By Meredith Wadman, Jennifer Couzin-Frankel, Jocelyn Kaiser, Catherine Matacic Apr. 17, 2020 , 6:45 PM
_____________________________
April 23, 2020 Increased death rates, increased cases
Today's newspapers are full of angry reports about how cases and deaths could have increased so rapidly, while what is actually happening is improved testing of people - living and dead - not previously identified as having COVID-19. I believe it will get much worse before it gets better. Particularly in nursing homes, dormitories, and other places where close-quarters living and working has continued.
April 22, 2020
The New York Times just updated their web site showing rates of reported COVID-19 cases and deaths by country, state, and city (MSA) which is updated daily. This is my go-to location for up to date rates. They are now using the most recent week of data (versus five days, previously) and recentered all their plots to start when a country or state had 200 cases (or 100 deaths) instead of ten.
There is an excellent overview of sources by Vivian Ho, Kirstin R.W. Matthews, and Heidi Russell, from the Rice Baker Institute. I first learned about this from The Incidental Economist blog by Austin Frakt. I recommend you choose which sources you want to review for your update.
One anecdote reflecting my own experience is revealing:
Yesterday I spoke for 20 minutes with someone working closely with an estate attorney. Several things surprised me. This person ("Jane") said that the lawyer in the Boston area was swamped by demands for living wills and do not resuscitate (DNR) orders (covering what to do when faced with the choice of being on a ventilator, for instance), updated wills, trust tax forms (no extension granted for these) and particularly assistance to households trying to get death certificates from the state.
Jane revealed two nursing homes in the area that have not yet gone public with the surge of deaths they have experienced because of fears over negative publicity.
Jane spoke of several people who died in nursing homes who were not yet reported to the state because when a death occurs at home or in a minimal care nursing home a death certificate requires verification by a coroner, and coroners are overwhelmed just now. The coroner must decide whether an autopsy is needed, and what samples should be taken before determining the cause of death. This is causing a serious delay. This leads me to believe that deaths in total and deaths attributed to COVID are being understate in some places in the US, and that more reliable estimates will want to look at deaths by age this year versus over past years.
These unreported deaths are consistent with recent reports in the media about new tests of samples from deceased bodies are turning up new cases of SARS-COV-2 not previously recorded.
April 22, 2020 Nursing home rates skyrocket.
Yesterday, April 21, the Boston Globe published a site for Massachusetts nursing homes that reporting confirmed cases by named. Unfort6unately they only have three tiers: <10, 10-30, and 30 or more. The results are stunning. A total of 228 Nursing homes are reporting cases of COVID, out of 338 in the state (56%). The data is to granular to calculate
My own calculations using the Massachusetts nursing home data as of April 22, 2020 posted on the Boston Globe web site suggests that among those reporting at least one confirmed COVID case, the average rate of confirmed cases is 15% or more of all residents, much higher than the population averages reported for older age groups.
I commend the Massachusetts Department of Public Health for publicly posting its rates of testing, new cases, rate of hospitalization, and deaths each day. Rates by race and place of death are reported. Also interesting is the detailed PPE supplied by region. Rates of N95/KN95 and other masks still seem distressingly low in the state.
I will mention that the number of COVID tests done per day has remained constant at approximately 5,000 since March 24, and that the very high positive test rate - average of 26% over the past five days - suggests that there remains a very large number of infectious cases not being identified at existing test levels.
April 22, 2020 Humor and misinformation
I was trying to track down a legitimate post mentioned on Facebook and had reason to view a variety of Facebook sites ridiculous postings. Some of the claims so outrageous as being hilarious. Here is one of my favorites:
"It will be extremely important for the truth about the events of September 11th, 2001 in New York to come out one day, including the truth about the use of a Directed Energy Weapon to "Dustify" the buildings. I hope and pray."
I was originally going to post several more ridiculous claims. but they were gone!
When I went back to Facebook to copy them, they had been removed. Plus, in two cases, I saw notices from Facebook that they had fact checked some consumer posts, and inserted a link to discuss why certain key statements were false. Hallelujah! Great to have Facebook start actually policing postings and repostings for accuracy.
April 21, 2o20
I was forwarded an interesting article about hypoxia in the NY Times that is worth a read.
The Infection That’s Silently Killing Coronavirus Patients: This is what I learned during 10 days of treating Covid pneumonia at Bellevue Hospital. By Richard Levitan, April 20, 2020
It describes how COVID19 induces hypoxia and recommends the use of a pulse oximeter as a low-cost route to early identification of COVID pneumonia. One of the striking findings in the article is that the normal signal of breathing problems (a build-up of CO2) doesn’t happen with COVID-19, so that hypoxia can progress quite far, without the person realizing that anything is wrong – hence the value of proactive monitoring of blood oxygen levels.
Widespread pulse oximeter testing could be very significant for our ability to manage COVID-19 during the ‘dance’ phase, by changing the ratios at several important points:
- Reduced R: Earlier detection of COVID19 cases through early identification of hypoxia, even before other symptoms have developed has the potential to increase the ability to isolate earlier and reduce the infection rate.
- Reduced % of cases needing ICU beds or ventilators. Earlier detection of hypoxia would allow more routine treatment and less need for oxygen or intensive care, reducing the pressure on ICU beds and on ventilators. The NYT article suggests that better treatments alone – e.g., better positioning of the patient for better breathing could reduce ventilator need in the first 24 hours by 75%.
- Reduced mortality rate. The NYT article doesn’t speak to this directly, but it is suggestive that a major reason for the high mortality rates for individuals without other underlying conditions is that the hypoxia has progressed to dangerous levels before seeking treatment. If so, avoiding dangerous levels of hypoxia might dramatically reduce mortality rates for otherwise healthy individuals without underlying conditions.
April 20, 2020 UK report on exit strategy
Interesting UK report from Ian Mulheirn, Executive Director and Chief Economist, Institute for Global Change.
PPT: Suppression Exit Strategies: Options for Lifting Lockdown Measures in the UK
Tradeoffs presented, but no mechanism for choosing. No discussion of ameliorating drugs (preventive, symptom control, treatment) prior to a vaccine.
April 20, 2020 Humor/Art
Covid video from an art historian
April 20, 2020 Masks
The US continues to be woefully unprepared for the volume of personal protective equipment (PPE) needed and is still totally failing to keep up with the urgent need. Here is one telling quote from Dr Steve Corwin President and CEO of New York Presbyterian Hospital speaking to CNN on April 6, 2020:
"We can't make that mistake again. I know the next crisis will be different than this one. But let me just give you a statistic, pre- crisis, we were using 4,000 masks a day of all sorts. Now we're using 90,000 masks a day."
Given that there are 2650, staffed beds at NY Presbyterian, that implies 34 masks per bed per day. Official guidelines are for hospital workers to put on a new mask each time you enter a patient's room, which is a lot of masks for each health care worker and each patient. Fortunately some areas have figured out how to sanitize and reuse some N95 masks, but the costs of doing this may exceed the costs of making a new mask, which with bulk production are fundamentally very inexpensive. The magnitude of the need is still unprecedented.
This following table calculates the magnitude of the mask problem for New York state, Massachusetts, and the nation assuming the same rate of need as NY Presbyterian Hospital in early April, before the peak need in NYC.
|
NY Presbyterian hospital |
All New York state hospitals |
All Massachusetts hospitals |
All US Hospitals |
| total staffed beds |
2,650 |
53,000 |
15,193 |
924,107 |
| masks per bed |
34 |
34 |
34 |
34 |
| masks per day |
90,000 |
1,800,000 |
515,989 |
31,384,766 |
| days per month |
30 |
30 |
30 |
30 |
| masks per month |
2,700,000 |
54,000,000 |
15,479,660 |
941,542,981 |
Governor Cuomo has asked new York hospitals to add another 20,000 emergency beds, which increases the demand even more. These calculation suggest a need for more than a billion masks per month to meet the US hospital demand for masks.
Notice I am not talking about N95 masks, but "all sorts of mask", just like Dr. Corwin. This calculation ignores the additional masks needed for dozens of other occupations (police, firefighters, public health, pubic transport, food workers, pharmacy workers, and other essential workers). Given their numbers, this easily adds another billion masks per month. Then there are ordinary citizens: if each citizen wanted to use new three masks per month, that would add another billion face masks. These uses quickly triple the number demanded nationally: 3 billion masks per month, or 100 million masks per day.
These levels of demand would require a thousand plants each producing 3 million masks a month, just for serving the US. While a charity event like the Boston Patriots owner flying home 1 million masks from China that were shared between hospitals in NYC, Rhode Island, and Massachusetts, was helpful, achieving a day’s supply at best for the three regions, a much bigger concerted effort is needed. Masks are not expensive, this could be done for perhaps a billion dollars per month once scaled up. That is only $3 per American per month. We can do that.
Obviously a great deal of other PPE equipment is also needed. I need not make the calculations here.
We need the federal government to immediately use its emergency wartime powers to ensure that US industry is turned to producing these supplies at prodigious rates, not just rely in imports and voluntary private businesses to supply the need. After resisting the need for widespread mask wearing, it is time for the US to take this step before we consider partially reopening the economy.
April 19, 2020 COVID
It is clear that the US is not yet testing enough people for COVID-19 virus or antibodies. Here are two good links on the subject.
NY Times "Coronavirus Testing Needs to Triple Before the U.S. Can Reopen, Experts Say" By Keith Collins April 17, 2020
The Atlantic. A New Statistic Reveals Why America’s COVID-19 Numbers Are Flat by Robinson Meyer/Alexis C. Madrigal April 16, 2020
April 17, 2020 COVID
New BU working paper draft is posted here.
THE EARLY TOLL OF COVID-19 ON JOB AND INCOME LOSSES: VULNERABILITY BY OCCUPATION
Randall P. Ellis and Giovanna Marcolongo
Boston University, Department of Economics
April 17, 2020
Key message: Early PPP funding does not target the occupations most affected by the COVID-19 shutdown
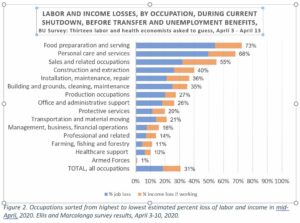
Figure 2 summarizes the key findings of a new poll of 13 labor and health economists from April 3 to April 10 conducted by the authors about rates of job and income loss of employees by occupation (including seasonal and less than full time workers).
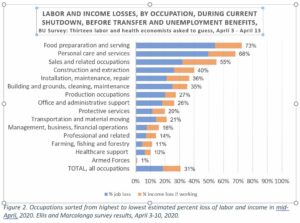
Overall, we calculate that the two-month income losses from the pandemic are $485 billion and argue that the most impacted occupations may be least able to benefit from the PPP loan program.
See the short paper linked here for more.
_____________________________________________________________________
I have shared a lot of articles and blogs on COVID-19. This BUHealth post puts them all in one place, with updating at the top.
Favorite links if you have not already viewed them.
Tomas Pueyo's March 19 article in the Medium: Coronavirus: The Hammer and the Dance.
The best source of up-to-date statistics I have found is on COVID19 is WorldoMeter.info/coronavirus. which gives daily updates and documents its sources.
COVID-19: An illustrated scientific summary 8 minute video
New York Times interactive figures are updated daily for the world and individual US states.
April 14, 2020 Herd immunity
Jeff Howe from the Boston Globe on April 11, 2020 summarized Harvard epidemiologist Marc Lipsitch modeling in a very direct, if unpleasant way. It is worth a read if you want to know what a top epidemiologist thinks.
"This is the simple, scary math that Harvard epidemiologists Marc Lipsitch and his colleague Yonatan Grad have tried to convey in a series of recently published papers: If each person infected with COVID-19 disease in turn infects three more, as we now think, then in order to bring the disease to heel, Grad says, two of those people must already be immune."
Currently we are hunkering down with less than 3% of people ever infected everywhere.
The figures in the Boston Globe article are easier to interpret than the three linked academic papers. Worth a sobering read if you care to.
This opinion piece by Marc Lipsitch in the NYTimes on 4/13/2020 is on a similar vein, and also presents evidence on how well people acquire immunity from exposure. Immunity appears not to be complete but only 80 – 90%.
My own belief is that the epidemiologists are perhaps too pessimistic about the assumption and implications. My reading is that good masks (see earlier posts below on Stanford study) reduce infection rates by 70 to 95%, so if everyone wore masks routinely, and also washed hands regularly, the infection rate need not multiply as rapidly as modeled for much of the population, which they max out at a 60% reduction. This points to the importance of high quality, comfortable and hence widely worn, personal protective equipment (PPE).
The biggest short run hope is not vaccination, but PPE, physical distancing, crowd avoidance, and above all effective palliative and treatment drugs so that the infectiousness and death rates can be brought way down. As an analogy, we have never found a fully effective vaccine for malaria, and malaria is still a potential risk even in the US (and Spain and Italy), but we now have very effective prevention methods and treatments for it, so that rates of reinfection are low here and deaths and serious cases rare. The Jeff Howe 4/11 Boston Globe article mentions that 40 different drugs have been approved for clinical trials in the US. These are treatment drugs, not vaccines. If at least one of them is highly effective, then we would free up a lot of ICU beds, reduce pain and deaths, a make us all a lot less fearful of the disease. By focusing on already existing drugs, we have a much better chance of one becoming available sooner. This give me hope, because the infection simulations and impacts on the economy do not look good without this.
Also giving me hope is that several health economists are coming out with behavioral models that may do a better job at building in feedback loops than the existing epidemiological models that I have seen.
Hope for a COVID-19 vaccine — a conversation with David Spiegel
April 11, 2020 Birdwatching in Newton
Today my wife and I took our dog for a walk at Brayburn Country club and saw eighteen species of birds. Most notable were a pair of bluebirds, a pair of green-winged teal, and two magnificent male wood ducks. Also seen today were turkey vulture, red-tailed hawk, mallard ducks, Canadian geese, chipping sparrow, house sparrow, grackle, starling, mourning dove, chickadee, robin, goldfinch, white-breasted nuthatch, red-bellied woodpecker, chestnut-sided warbler, and at our feeder pine warbler, two turkeys, (including a Tom on full display), cardinal, junco, blue jay, house finch, gray squirrel, and chipmunk. Fun to see 20+ species on a casual day near home. Our winter viewings since COVID-19 quarantine is now 36 species.
April 10, 2020 Happy Holidays to all!
700 inspiring children's voices from Italy: https://youtu.be/MZWmikiJVIQ
I pass along the holiday greetings of my friend Shuli Brammli of Israel
Dear Friends,
This week we are entering a period when the three religions are celebrating their spring holidays. One by one we celebrate Passover, followed by Easter and then by Ramadan Kareem of our brothers the Muslims. We don’t know much yet about the consequence of this Epidemic that we all experience. But one fact is undeniable. We all live in one small world and there is no other world for us. It is too small to be ignored. I hope that we will be smart enough to learn the lesson from this, and that we will be kinder to each other and compassionate, promote social support and mutual guarantee within our society as well as between our countries. I wish you all the best for you and your beloved ones.
Happy holidays
Shuli
April 10, 2020 BU to Open Fenway Campus to Pine Street Inn homeless shelter employees
I was proud to see BU offering their empty dorms to the homeless shelter staff, some of whom are themselves homeless.
Now is a good time to give to Pine Street Inn (homeless shelter) and the Greater Boston Food Bank (wholesale food pantry) donations or your own local shelters and pantries.
April 10, 2020 More on job impacts of COVID pandemic
There is an important article by Noam Levy at the LA Times that is worth a careful read.
Here are a few sentences.
"Primary care doctors have seen a big uptick in telehealth visits — a move widely hailed by public health experts. However, the fees for these services are often lower than for office visits. Many physician practices have seen in-person patient visits drop 50% or even 75%. That has left physicians struggling to stay afloat and forced growing numbers to consider laying off staff or even closing their doors. Nearly 8 in 10 primary care clinicians in one recent survey reported their practice is under “severe” or “close to severe” strain due to COVID-19, the disease caused by the coronavirus.
Stunning survey results from a Seton Hall Sports Poll conducted on Thursday.
"Seventy-two percent of Americans said they would stay away from a sports event if it were held before a vaccine is developed. Even if the seating arrangements allowed for social distancing, just 12 percent would be comfortable with that setup."
Also revealing was yesterday's Boston Globe report on tech industries in Massachusetts.
A few selected quotes.
"Toast, the maker of popular software and systems used by the restaurant industry, said late Tuesday that it was laying off over 1,000 employees, reducing its workforce by about half through layoffs and furloughs. The company said that restaurant revenues have declined by 80 percent since state and local officials began shutting down businesses nationwide, and “our success is tightly coupled with the success of the restaurant industry."
" Lola.com, Zipcar, Hopper, and Wanderu have all cut back workers as travel restrictions have decimated the industry. At Logan Airport, the number of passengers fell by 93 percent between March 23 and 29, compared to the same period last year, according to the latest Massport data."
This NY Times article on inequality also speaks to the huge inequality of burdens.
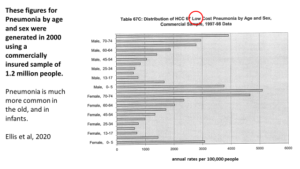
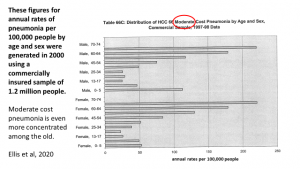
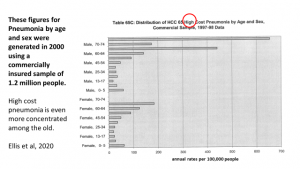
April 8, 2020 JAMA Network Open paper published!
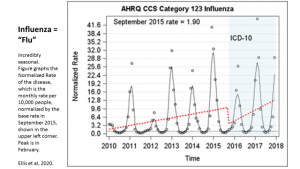
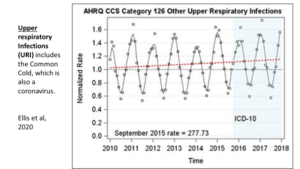
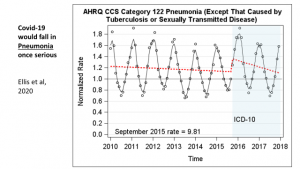
Although tangential to this COVID blog, the big news for me on April 8 was the appearance of my first first-authored paper in JAMA. It is worth a click if you understand the importance of disease tracking over time.
JAMA Network Open (Open means it is free to all viewers)
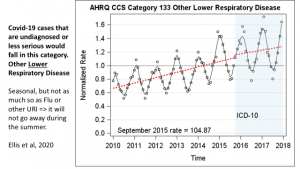
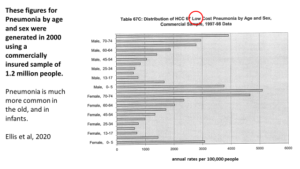
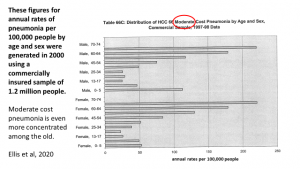
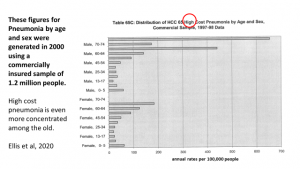
Original Investigation Health Policy April 8, 2020
Randall P. Ellis, PhD; Heather E. Hsu, MD, MPH; Chenlu Song, MA; Tzu-Chun Kuo, PhD; Bruno Martins, PhD; Jeffrey J. Siracuse, MD, MBA; Ying Liu, MA; Arlene S. Ash, PhD
Question Was the US transition from ICD-9-CM to ICD-10-CM in October 2015 associated with dramatic changes in diagnostic category prevalence in various classification systems?
Answer: YES. See the paper’s figures to see how much.
It has been a long time coming, but here it is! We didn’t like the title either, but JAMA insisted. This is the first publication from our ICD10 project. We use 1.2 billion data points for the figures, which are the best thing to look at.
April 8, 2020 Humor #2
Introverts and Extroverts
Humor #2 in figures.
Words of wisdom from Richard G Ellis:
Stay inside + Stay healthy = Stay Stealthy!
Interminable meetings.
April 7, 2020 Economic effects.
The Economist, March 25, 2020:
https://www.economist.com/finance-and-economics/2020/03/25/how-to-pay-for-the-pandemic
Economic Cycle Research Institute (ECRI), April 4, 2020:
https://www.businesscycle.com/ecri-news-events/news-details/business-cycle-economic-cycle-research-ecri-recession-recovery-lakshman-achuthan-anirvan-banerji-a-nasty-short-bitter-recession
McKinsey Insights: https://apple.news/A8W8neEEvNTGaecv19reqUA
April 6, 2020 pets can get infected
There is now significant evidence that pets, such as dogs and cats can become infected with SARS-CoV-2, however no evidence yet over whether they can infect humans through the air. But it seems likely. Here is the evidence from the American Veterinary Medical Association (AVMA). I personally will not stop petting our dog, and will consider her part of the family who is at risk of exposure if any of us become ill. We no longer let her get close to any other dogs or people, so she is like other members of our family.
_____________________________________
April 6, 2020 Effectiveness of different types of homemade mask materials.
Stanford medical school site. Key figure.
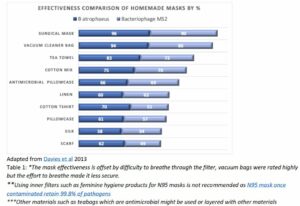
Adapted from Davies et al 2013
________________________________-
April 6, 2020. How to sanitize masks against viruses.
The link on the previous posting from Stanford includes advice for achieving medical quality sterilizatoin of N95 masks. Here is the key table.
Their key finding is don't use bleach or alcohol to sterilize masks since it can change how well they filter or the difficulty breathing. heating anything in an oven to 160 for 30 minutes will kill the virus.
My reading is that for cloth masks, where you want adequate but not surgical safety, any of the following should work
Running them through a load of wash, where the soap will remove the germs to practical levels.
Put them in a dryer at high temperature for ten minutes.
Put in hot or boiling (not recommended for many rubber or stretchy attachments, however).
Leaving things out in the direct sun for a half hour works because of UV light.
Or leaving them unused for a five days will also kill COVID germs (but not necessarily other germs).
The other key advice is not to reuse or handle used masks. Treat them as if they are used tissues. If you have been around anyone who is infectious, and your mask has done its job and filtered/caught any bad germs, then you don't want to be touching the germs or reattaching them to your face. best is to have several and just routinely use a different one once you have been out with one.
April 6, 2020 Sewing your own fabric mask from the NY Times
This requires having a sewing machine to make several well.You probably have a friend or neighbor happy to give or sell you one for a donation to a good cause.
In a pinch, the following simple technique could also be effective if bulkier in areas where it is not too hot.
Find a 100% cotton T-shirt and a black binder clip. Put the whole T-shirt over your head and use the binder clip (or a safety pin) to shrink the size of the head hole to be snug around your nose and mouth, leaving the rest of the shirt just hanging around your neck. When done visiting the store, throw shirt in a plastic bag, wash your hands, and be sure to launder the t shirt before the next use. Keep several T-shirts handy.
Any face mask will only work if you actually wear it... Half (?) of its effectiveness is probably from the reduced ability to touch your mouth and nose. Wear glasses or goggles to also reduce eye touching.
__________________________________
April 4, 2020
The media is full of predictions of the date on which rates of hospitalizations, and deaths will peak. Many of them are informed by the model from IHME, the Institute for Health Metrics and Evaluation, which is led by Christopher Murray, a well regarded health economist and MD, now an adjunct professor at the University of Washington. He is best known for his work calculating the burdens of disease for WHO and the World Bank. IHME are updating their predictions for COVID-19 every few days.
There is a research paper in draft form linked here.
I think this comment below on that paper sums up well the weaknesses of this method. Murray uses a simple parametric model, and assumes that the rate of new infections will be a symmetric Gaussian sigmoid function. There is no evidence that the decline will be symmetric with the rise, and indeed the evidence from South Korea is that it does not return to a zero rate, but rather to a low, but still growing rate of growth. So I do not place a lot of faith in the predictions other than that in the short term we are in for some very difficult times. States that started lock down earlier will face less exposure. Those that have yet to start, could be in for a much higher mortality. For reasons discussed below, I do not believe the China rates of extremely low deaths recently are entirely reliable. There is reason to believe that they have been concealing deaths.
While it is easy to be critical, no one really knows what the right hand tail will look like, and I do not know any other model that is worried about short term forecasts as much as this one.
The bottom line of their model, as of today 3/4/2020 at 12:49 pm EST is that they forecast that the US hospital bed demand will peak on April 15, 2020
Resources needed for COVID-19 patients on peak date
All beds needed: 262,092beds implying a Bed shortage of 87,674 beds
ICU beds needed: 39,727beds implying an ICU bed shortage of 19,863beds
Invasive ventilators needed: 31,782 ventilators
He forecasts that the number of deaths will peak one day later at 2,644 per day. With eventual deaths by August 4 of 93,531.
At his last update three days ago, he raised his estimated beds needed and deaths. the web site says that it will be updating its model and predictions today, April 4.
April 4, 2020
It is only a newspaper report, but the 3/4/2020 Boston Globe had an interesting article about funerals in China, which has been receiving some attention. China is making it hard to attend an count deaths through this normal means. So people have been using other methods.
https://www.bostonglobe.com/news/world/2020/04/03/china-curtails-memorials-during-tomb-sweeping-festival/QUBuvZg0jVntNTk9SqcQGO/story.html
Below is the relevant text to me. Two different estimation techniques both give much higher estimates of death. Note that the current death count in China is still only 3,326. Only slightly more than Iran, another country that people question: how could they be so successful?
“Long lines have been forming at funeral homes in Wuhan over the past two weeks, as family members have been informed they may collect their loved ones’ remains ahead of Tomb-Sweeping Day. Some waited six hours to collect an urn, then the ashes.
The Hankou Funeral Parlor’s crematorium was operating 19 hours a day, with male staff enlisted to help carry bodies. In just two days, the home received 5,000 urns, the magazine Caixin reported.
Using photos posted online, social media sleuths have estimated that Wuhan funeral homes had returned 3,500 urns a day since March 23. That would imply a death toll in Wuhan of about 42,000 — or 16 times the official number. Another widely shared calculation, based on Wuhan’s 84 furnaces running nonstop and each cremation taking an hour, put the death toll at 46,800.
Wuhan residents say the activities belie the official statistics. ‘‘It can’t be right . . . because the incinerators have been working round the clock, so how can so few people have died?’’ a man, identified only by his surname of Zhang, told Radio Free Asia.
US intelligence agencies have reportedly concluded that China’s numbers are much lower than they are in reality.”
Let me note that these reports on urns and cremations might also be biased, reflecting misinformation. I won’t speculate on how or why.
I myself look at South Korea as the country most likely to have a reasonable trend. They are showing a reduction to less than new 100 cases a day, with deaths hovering around 10 per day. Even scaled up for the US, that is a level that buys us time until we get a virus. That seems credible to me.
April 3, 2020
This 8 minute video produced gives the best scientific overview of COVID19, and I am sending it out to my full set of BUHealth recipients. It is accessible and would be understood even by an intelligent child, although complex topic.
As before, I am posting my other updates on a single blog site to not overwhelm people
COVID-19: An illustrated scientific summary
A Yale grad student explains the basic biology of COVID-19 infection and transmission — and why social distancing measures can flatten the curve.
_________________________________
April 3+, 2020 Humor
Links that will make you smile.
Two more fun links.
Horse with no name (30 seconds)
Testicles (30 seconds)
Two Facebook links:
Cute puppy. (2 minutes)
Italian pianist. (3 minutes)
____________________
April 3, 2020
Yesterday was a day of much bad news. First an Italian colleague and health economist stated and provided further support today, that there is evidence from Italy that health care workers who are believed to have had COVID and recovered, have become reinfected and showing new symptoms. This was also supported by news in the NY Times (source not provided) of reports coming in from Wuhan that an estimated 5-10 percent of people are becoming reinfected with the virus, after seemingly recovering.
The other bad news is that the articles in today's papers that the current COVID test used for current infections appears to have a 30% false negative rate. This is really bad because it means that after testing and sending people home, 30% may still have COVID.
More bad news is that two people I spoke with in our summer town in Maine thought that the presidents financial stimulus would not be of any value to them, for different reasons. So as I have worried, the very lowest income citizens may not be helped meaningfully by the measures taken to date.
My own "back of the envelope" calculations using my own guesses about rates of job loss and lost income suggest that US income during the shutdown may have fallen by 40%, with an even larger drop in spending. This is unheard of in previous recessions.
_________________________________
April 1, 2920
This posting from "TheLawyerBubble", which I do not know, focuses on cited quotes by Donald Trump over time which clearly show that Trump repeatedly lied to the US public and caused delay which is very costly to the US. It will mostly interest Americans, but highlights the importance of good leadership.
How many will die from Donald Trumps Lies?
_________________________________
March 31, 2020
John Burn-Murdock has been generating a series of excellent figures on COVID trends by country. There is a rich set in this series of Twitter feeds today. I recommend them to you.
This confirms what others have said, that there is no relation of infection rates to size of population across countries, at least for the low rates now. Ultimately population size will matter, but recall that even in the three countries with the highest rate of infections (Italy, Spain and Switzerland), the rate is only just over 150 per 100,000 which is .15%. So the saturation that slows down the rates of growth is not yet in effect. The US rate is only 39 per 100,000, which is .039%.
It is not the absolute levels that should make us scared but rather their rates of growth. If they double every 3 days, then in 30 days they will have doubled ten times and 2^10=1024. Multiply the above percentages by 1000 twice and you have everyone infected. Burn-Murdochs figures show no slowing down by population size, only by actions taken in some countries.
March 30, 2020
In case any readers are interested in doing your own empirical analysis of county rates of infectoin with COVID, the NYT might pick up if well done, they have just posted their entire dataset of county level cases and deaths from January 21 to at least March 29, 2020. Look here.
An article describing what has been posted is linked here.
Others have documented states and cities who have implemented guidelines and lockdowns. There are dozens of papers eventually to be written about all of this information.
RE
_____________________________
March 30, 2020
These New York Times interactive figures and interpretation from today's Upshot are excellent.
It is clear that Korea and China have done something critical by slowing the doubling rate to once per month or less.
The US is now the laggard. But the disease always spreads faster when entering a new area and rates are low. So what will matter is how they look in areas where there has been time to respond. In a few states there is encouraging news in that the rate of doubling has slowed down to about once every month instead of every two days in the worst cases.
RE
March 30, 2020 RE
I want to retract some of my enthusiasm in light of a link from a BU colleague.
https://blogs.sciencemag.org/pipeline/archives/2020/03/29/more-on-cloroquine-azithromycin-and-on-dr-raoult
While the news is on a larger sample of N-80, an article in today’s Science Magazine questions the reliability of the finding. It is still not a randomized controlled trial, and was done on a sample with a median age of 54, where a lower complication rate would be expected anyway.
My previous post is below.
________________________________________
March 30, 2020
Fabulous news just in from France. If validated, this could be a game changer for this COVID battle. N=80.
France Officially Sanctions Drug After 78 Of 80 Patients Recover From COVID-19 Within Five Days | The Daily Wire
_________________
March 30, 2020
There is also a key literature on the effects of hospital strikes on mortality. Cancelling all elective procedures and non-urgent care for COVID is a similar impact to a MD strike. This study from 2008 did a meta analysis of 156 studies of strikes from around the world, of which only 7 studies were considered high quality. These seven suggest that in every case an MD strike in the short run resulted in the same or lower overall mortality. They acknowledge that this is only the short run effect. But the cancellation of elective surgeries in the developed world tends to reduce other causes of death in the short run. Hard to build into models, but very real. Assuming zero or small negative change in the short run seems credible. More than a few weeks, who knows.
https://www.researchgate.net/publication/23311966_Doctors'_strikes_and_mortality_A_review
____________________
March 30, 2020
Growing evidence that masks are key to containment. thank you BU alum Jing Guo for these links and text.
Wearing mask also helps us to dance well in the long run before we all can get effective vaccine. I'm glad to see more articles about wearing masks these days:
https://www.sciencemag.org/news/2020/03/would-everyone-wearing-face-masks-help-us-slow-pandemic
https://www.nytimes.com/2020/03/27/health/us-coronavirus-face-masks.html?smid=em-share
___________________________
March 29, 2020
Everyone should be wearing masks when out of the home or around people at home who might be infected. Most of the west has been in error about not advocating their use. Here is a good video.
https://youtu.be/HhNo_IOPOtU
BEST OVERVIEW.
Tomas Pueyo's COVID:Hammer and the Dance is the best overview of the issue from early this week.
https://medium.com/@tomaspueyo/coronavirus-the-hammer-and-the-dance-be9337092b56
The following University of Chicago article is also interesting and has much higher costs of the pandemic than some others. It does a cost effectiveness using the value of a statistical life.
https://bfi.uchicago.edu/working-paper/2020-26/
_______________________________
3/27/2020
The best source of up to date statistics I have found on COVID19 is WorldoMeter.info/coronavirus.
I visit it daily.
In WorldoMeter, I especially recommend the figures using the log scale on the vertical axis, so that you can quickly calculate the days before doubling or sadly the days before a ten fold increase.
As of March 27, the World is doubling every six days in terms of cases and deaths, while the US is doubling every 3.5 days. If this pattern continued for two months (60 days), then the cases and deaths from COVID19 in the US would exceed the US's population. If we slow down to the world rate of increase the US rate would still increase by the multiple 2^10 = 1024. If the US continued at this rate, every American would be infected in 60 days (A 32,000 multiple). If we assume the US only slows down to the current world rate then the following numbers emerge. This is not a prediction, only a calculation.
|
World |
USA |
|
|
|
|
|
| Doubling time (T) in last week |
6 days |
3.5 days |
|
|
|
|
|
| Times doubled in 60 days (50/T) |
10 |
|
|
|
|
|
|
| Multiple after 60 days (2^(60/T)) |
1,024 |
|
|
today |
60 days |
Today |
60 Days |
| cumulative cases |
596,366 |
610,678,784 |
104,126 |
106,625,024 |
|
|
|
|
|
| cumulative deaths |
27,345 |
28,001,280 |
1,696 |
1,736,704 |
|
|
|
|
|
| Calculations based on extrapolating most recent growth paths for 60 days |
| Source: Worldometer |
|
|
|
|
In all of World War II, there were only 405,000 American deaths.
For President Trump to assert that the worst is over and that we should reopen everything on Easter would be equivalent to announcing that WW II was over two months after the US entered the war.
3/27/2020
Best humor.
On Mar 27, 2020, at 7:02 PM, Randy Ellis <ellisrp@gmail.com> wrote:
________________________________________
I am impressed with how the Atlantic is publishing great overviews of this pandemic.
The four possible timelines for life returning to normal
The coronavirus outbreak may last for a year or two, but some elements of pre-pandemic life will likely be won back in the meantime. Read in The Atlantic: https://apple.news/AxwhNr30XQiWDDkWSUTvJFw
_______________________________
There has been a lot of misinformation about how seasonal COVID19 is likely to be. We have no prior information, so many are looking to the seasonality of Influenza (the flu). But more informative may be that of pneumonia, since COVID mostly causes lower respiratory infections (pneumonia), not upper respiratory ones, like the flu. Some work I am doing with a team has looked at monthly diseases rates per 10,000 people on 1.2 billion US monthly observations. These four pictures tell an important story.
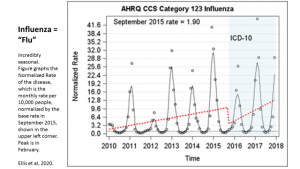
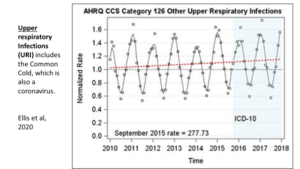
If it were in our data, COVID would likely be classified into this CCS disease category and are likely to have similar seasonality.
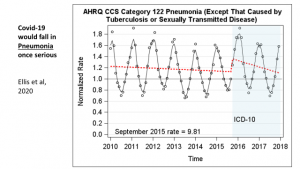
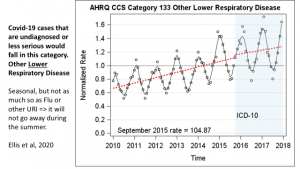
Age patterns of prior high cost pneumonia cases also display a pattern similar to COVID, and seasonality by age would be possible with our very large datasets. The following figure is based on old data, and shows rates per 100,000 people. Something similar could be done with our newer data. It would be even more interesting with All Payer Claims data, which we hope to have available for a sample of states already. Notice that older Americans have much higher rates of treated infection, and this is much more likely to be high cost when they are infected.